Keep Your Back On Track
Claim a $49 New Patient Appointment!
Specialized Consultation
Deluxe Exam
Extensive Report of Findings
Over $200 VALUE
It's time to start living without pain!
About Our Practice
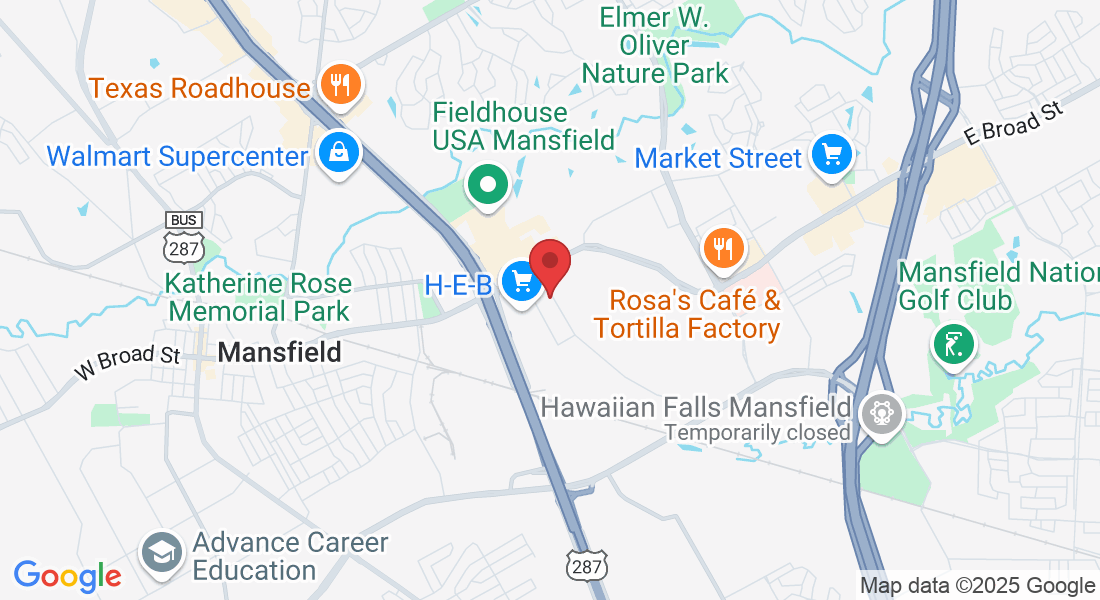
At Spinal Decompression Center, we specialize in relieving pain in patients with disc problems. Dr. James has successfully treated thousands of patients with low back pain, pain radiating down the legs, neck pain, pain into the arms and aching and soreness in joints. We use a combination of therapies, including cold laser treatment, decompression therapy, electric muscle stimulation, cold and heat to reduce your pain. Chiropractic adjustments re-align the vertbrae to relieve nerve pressure that can cause pain. Chiropractors spend many years studying muscular and skeletal health to offer a range of treatments. Our expert approach means you'll see the same practitioner every time, and we'll always do our best to explain how, and why, your treatment can help.

"When I first came to see Dr. James, I could not walk from the living room to the kitchen because of the pain in my low back. After my first few treatments, my pain went from a "10" on the pain scale to no pain at all."
• John E.
Claim A $49 New Patient Appointment!
Enter your details below to claim voucher